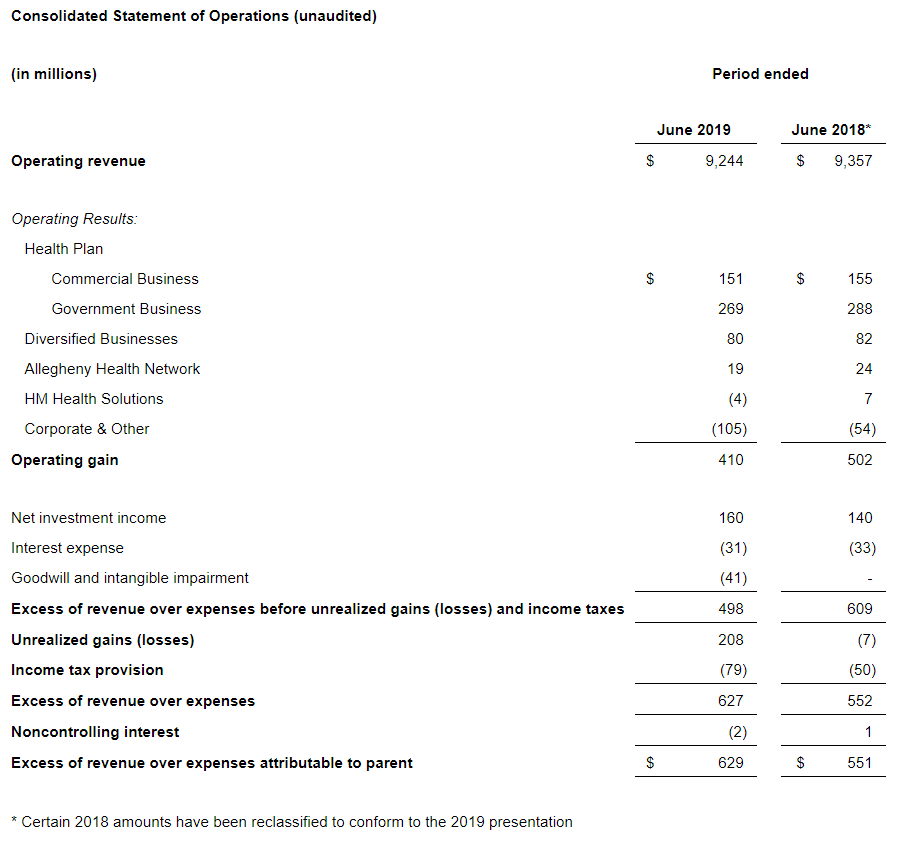
Highmark Health announced Thursday the financial results for the first six months of 2019, reporting an excess of revenue over expenses of $629 million and an operating gain of $410 million.
These results are due to the strong performance of most business units, notably Highmark health plan’s strong commercial and government business results, driven by continued focus on value creation initiatives; stable results in the Diversified Business due to continued strong performance in the dental business and Visionworks, as well as sustained positive margins at HM Insurance Group; and operational improvements at Allegheny Health Network.
Total consolidated revenues were $9.2 billion for the first six months of the year. Highmark Health maintained a strong financial profile with nearly $8.3 billion in cash and investments as of June 30, 2019, an increase of nearly $430 million since December 31, 2018, and net assets of more than $7.4 billion as of June 30, 2019.
“We have continued to make significant progress in the purposeful execution of our strategy. No health organization in the country is doing more than Highmark Health to strategically invest in bringing new types of access and new clinical resources to the people and communities that we serve,” said David Holmberg, president and chief executive officer. “This will not change. In fact, we are staying the course, and executing on our game plan to provide more health care choices in the community and to build a more effective and affordable community-based health care network. Our go-forward strategy continues to be focused on re-inventing health care – building an operating model that delivers differentiated value, and creates a remarkable health experience – for our customers, members and patients across the full spectrum of their needs. Our commitment remains the same: getting health care right.”
“Highmark Health extended the positive financial momentum we have experienced during the last two years through the first six months of 2019,” added Karen Hanlon, chief operating officer and treasurer of Highmark Health. “We continue to see strong performance across most business units, with a consolidated operating margin of more than 4 percent — which we believe is living proof that our integrated delivery and financing system model is working. We are particularly pleased that Allegheny Health Network sustained its financial momentum during the first half of 2019, reporting positive operating margins for nine consecutive quarters. Families and individuals in western Pennsylvania, including Highmark Health Plan members, are choosing the high-quality, affordable services that Allegheny Heath Network provides.”
The Highmark Health Plan reported an operating gain of $420 million for the period ended June 30, primarily driven by effective performance in the government business, a continued focus on clinical transformation activities, and solid membership retention.
Highmark’s commercial business delivered an operating gain of $151 million for the first six months of the year. Through the health plan’s focus on clinical transformation initiatives – aligned with the same efforts at Allegheny Health Network – the organization continues to build momentum on reducing care costs and delivering value to its customers.
Highmark’s government business – which includes Medicare Advantage, Affordable Care Act (ACA), Medicaid and small group segments – also contributed to the health plan’s overall performance with gains of $269 million. This is due to the implementation of care management programs and designed benefits that encourage the use of lower-cost, higher-quality care options. These efforts result in savings for Highmark members through smaller premium increases – or even decreases – for health plan products and have led to a more stabilized risk pool and more appropriate pricing, particularly in the ACA business.
The organization continues to see the positive results of its transition and transformation efforts in core health plan membership, which remains steady at more than 4.4 million Highmark members through June 30, with July 2019commercial renewal rates across the Western Pennsylvania region at more than 95 percent.
Highmark’s diversified businesses reported combined earnings of $80 million through June 30, which is even with prior year results, driven by continued strong performance by United Concordia Dental and growth in comparable store sales at Visionworks.
United Concordia Dental continues to perform well in both its government and partner business, delivering an operating gain of $52 million, an increase of $7 million from the previous year.
Highmark Health’s stop loss business, HM Insurance Group (HMIG), reported an operating gain of $25 million, a decrease of $19 million year over year. This decrease is largely due to a return to normalized margin levels after an exceptional prior year performance.
Visionworks experienced strong sales in the first quarter, consistent with industry trends, resulting in an operating gain of $3 million, an increase of $10 million over the previous year. This revenue growth, as well as the pending sale of the vision business, delivers on the multi-year turnaround plan that positions the business for continued success.
Allegheny Health Network delivered operating income of $19 million through June 30, a decrease of$5 million compared to prior year, while net income was $47 million, an improvement of $29 million over the same period last year, driven largely by improved investment income year-over-year and steady operating performance. As previously reported, AHN refinanced its capital debt structure through a $1 billion bond offering in August 2018, which is proving to be an essential contribution to the long-term stability and future success of the organization.
AHN’s positive operating performance, which has now extended over nine consecutive quarters, was driven by several notable factors, such as increased physician office visits, more effective business and clinical processes, a more complex case mix, and improved care coordination through its integrated electronic health record system.
For the six-month period ended June 30, patient volumes grew year over year in a number of key categories. Total inpatient discharges plus observation cases grew by 4 percent, reflecting the industry’s continued shift away from inpatient stays to observation stays. Ambulatory surgery center cases grew by 10.2 percent, while live births grew by 5.3 percent and physician visits exceeded 1.6 million, an increase of 11 percent over the comparable period in 2018.
Outpatient registrations grew slightly year over year, while Emergency Room visits and operating room cases remained flat.
HM Health Solutions, the organization’s information technology services company, currently supports thirteen Blue Cross Blue Shield plans in multiple states, servicing more than 10 million members.
HM Health Solutions delivered a slight operating loss of $4 million through June 30, due to continued investment in the platform’s technical capabilities to keep health plan member costs low and to further implement operating efficiencies.
HM Health Solutions transitioned more than 500,000 new members onto the platform as of June 30, doubling the total number of members served on the platform since the company’s launch in 2014.
Corporate and other expenses increased over prior year, driven primarily by higher non-operating expense in the first six months related to transformational investments being made to enhance our data analytics and internal corporate capabilities.
Source: Highmark Health




